What is HF?
Heart Failure (HF) is a very common problem in the United States. 1 in 5 Americans will develop heart failure in their lifetime.1 About 915,000 new patients are diagnosed with heart failure each year.1 It is the leading cause for adults over the age of 65 to be admitted to the hospital. The most common cause for a visit to the emergency room for someone with HF is fluid retention. In the past, HF has been referred to as ‘congestive heart failure.’ Though fluid overload is a very common reason people with HF come to the emergency room, it is not the only symptom of HF.
How the Heart Works
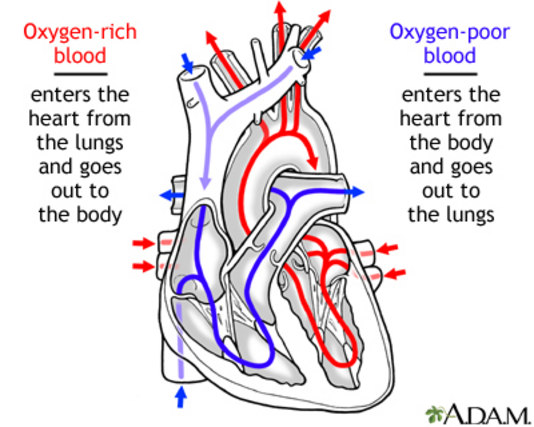
The heart is a four chamber organ in the middle of the chest beneath the breast bone. The four chambers of the heart are the left and right atriums, and the left and right ventricles. The purpose of the heart is to pump blood, rich in oxygen, to the rest of the body. The heart has its own blood supply. These coronary arteries surround the outside of the heart like a hand.
The right side of the heart receives blood from the body that is low in oxygen. It then moves it to the lungs to be refilled with oxygen and then returns to the left side of the heart. The left side of the heart moves blood filled with oxygen to the rest of the body, including other organs and the brain. The left side of the heart is a very strong muscle and is bigger than the right side.
When HF occurs it can affect the left or right side of the heart, or both sides.
What is Right-Sided HF: This occurs when the right side of the heart cannot pump the blood very well to the lungs. This can happen due to problems in the lungs or because the left side of the heart has become too big and is pushing on the right side of the heart. When the right side loses its pumping power, it can cause blood to back up in the body’s veins causing swelling in the abdomen, legs, and ankles.
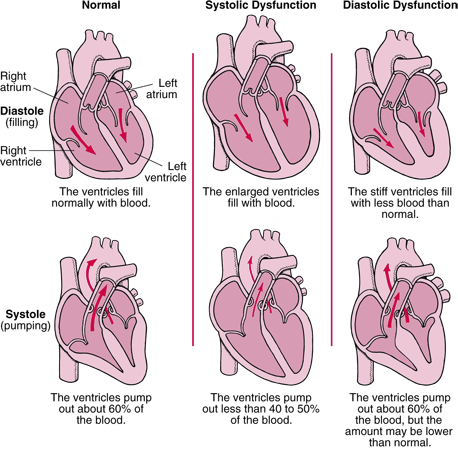
What is Left-Sided HF: There are two types of left-sided HF. The first type, systolic, is a pumping problem where the left side of the heart does not pump blood well to the organs of the body. This is due to a weak muscle. The left side of the heart can become weak from many reasons such as a heart attack, an infection, taking toxic medications, pregnancy, or a problem with one of the heart valves. There are also times when the cause is unknown. Simply put, systolic failure is when the left side of the heart cannot pump with enough force to push blood to the body.
The second type of left HF is called diastolic failure. Diastolic failure occurs when the heart is not able to rest between heart beats. This happens because the heart muscle has become stiff. Normally, the heart rests between each heartbeat and fills with blood. With this type of HF, the blood cannot fill the chamber well causing a lower amount of blood to be pumped out to the body.
It is important to understand the different types of heart failure, because the treatments will differ.
Causes of HF: The risk factors for HF include high blood pressure, high blood sugar, obesity, blood clots or plaque in the vessels, stroke, virus, a family history, and some types of toxic medications.
Symptoms of HF: The first step in treating HF is to know the symptoms so they can be treated quickly. Common symptoms of HF include:
- Having trouble thinking or being sleepy
- Feeling dizzy
- Feeling weak
- Unable to walk or do activity like in the past
- Being short of breath
- Cough
- Unable to lay flat
- Having chest pain or tightness
- Feeling heart beat fast
- Gaining weight
- Having abdomen swell or feeling sick to stomach
- Ankle swelling
- Cold hands and feet
How HF Affects Your Body: This section will explain the changes within your organs and how they cause the symptoms of HF. The symptoms of HF occur when the heart cannot pump the blood to major organs such as the brain, heart, stomach, liver, kidneys and lower limbs.
As the brain gets less blood it can make you feel confused. Weakness occurs as HF becomes more severe, and the heart cannot pump enough blood to meet the body’s needs. To try and help, the body moves blood from the arms and legs to more crucial organs such as the heart and brain. In turn, because the limbs receive less blood, you will often feel weak and tired even when just walking or climbing stairs.
Failure of the left side of the heart can lead to increased pressure in the veins of the lungs, forcing fluid into the little air sacs of the lungs. When these air sacs fill with fluid, air cannot enter leading to feeling short of breath, coughing, and wheezing. You may also have mucous or phlegm.
A fast heart rate may occur when the heart is trying to keep up with the body’s needs. The heart pumping faster and stronger may feel like fluttering in the chest or a heartbeat that feels fast or out of rhythm. This helps the body meets the demands for a short term, but causes harmful long term effects. The rapid heart rate prevents the heart from filling with enough blood, and thus less blood is pumped out to the body. A rapid heartbeat also more oxygen.
Rapid weight gain occurs when fluid builds up in the body. Because blood flow to the kidneys is less, hormones cause the kidneys to hold on to salt and water. This causes swelling in the feet, ankles, legs, hands, and abdomen. These hormones help meet the body’s needs in the short term, but cause harmful late effects on the body. This cycle causes more swelling in the body. You may be prescribed medicines such as ACE inhibitors to treat HF and/or high blood pressure. An ACE inhibitor works by blocking the effects of these harmful hormones.
Another part of the heart not pumping well is blood backing up to the stomach and liver. This causes a sick stomach, a feeling of fullness, or not wanting to eat.
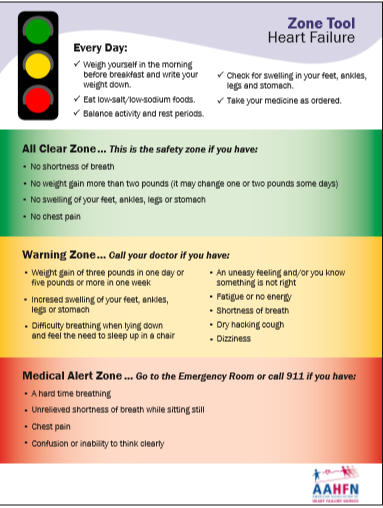
When to Call Your Provider or Nurse: It is important to recognize symptoms of HF and report them right away to your provider or nurse.
Many people wait to report these symptoms because they think they may go away, or are not severe enough.
Waiting will make the symptoms harder to treat and could possibly lead to an emergency room visit or hospital stay.
Your provider or nurse needs to decide if your symptoms can be treated at home, if you need to come into the clinic, or if you need to go to the emergency room.
Close follow up by your HF team is important. No one likes to go to the hospital, and recognizing symptoms early can help prevent a hospital stay.
The following Tool can help you recognize symptoms that need to be reported. The tool is divided into three sections
Green ( All Clear Zone): You are not experiencing any symptoms of concern. Continue to monitor yourself, weigh daily, follow your diet and fluid restriction, and go to regular checkups with your provider.
Yellow ( Warning Zone): You need to call your provider or nurse to report your symptom(s)
RED ( Medical Alert Zone): Go to the Emergency room if you have someone close by to take you right away, or call 911!
Heart Failure Stages, NYHA Functional Class and Disease Trajectory
It is important to understand the different stages of heart failure. HF symptoms and treatment may vary as HF progresses.
The staging system was developed by the American Heart Association and American College of Cardiology.
Your provider will work with you at each stage to help prevent and treat symptoms that may come with that new stage.
| AHA/ACC Heart Failure Stages | NYHA Functional Class | ||
|---|---|---|---|
| Stage | Description | Class | Patient Symptoms |
| A | Presence of heart
failure risk factors
but no heart disease and no symptoms |
||
| B | Heart disease is
present but there are no symptoms (structural changes in heart before symptoms occur) |
Class I (Mild) | No limitation of physical
activity. Ordinary physical activity does not cause undue fatigue, palpitation, or dyspnea (shortness of breath). |
| C | Structural heart
disease is present AND symptoms have occurred |
Class II (Mild) | Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in fatigue, palpitation, or dyspnea. |
| Class III (Moderate) |
Marked limitation of physical activity. Comfortable at rest, but less than ordinary activity causes fatigue, palpitation, or dyspnea. |
||
| D | Presence of
advanced heart disease with continued heart failure; symptoms requiring aggressive medical therapy |
Class IV (Severe) |
Unable to carry out any physical activity without discomfort. Symptoms of cardiac insufficiency at rest. If any physical activity is undertaken, discomfort is increased. |
Chart developed by C. Miller based upon below sources
Criteria Committee of the New York Heart Association. Nomenclature and Criteria
for Diagnosis of Diseases of the Heart and Great Vessels. 9th ed. Boston, Mass: Little, Brown & Co; 1994:253-256.
Hunt SA, Abraham WT, Chin MH, et al. (2005). ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult. Circulation 112 (12): e154–235.